
Penile implants were introduced into the marketplace over 30 years ago with the marketing of the three piece inflatable and the semi rigid rod almost simultaneously. Prior to that time, there was little interest in erectile dysfunction, little was known of the causes and epidemiology, and the treatments which were prescribed were in most cases unsuccessful. The rudimentary implants used prior to that time simply acted as inadequate splints, attempting to maintain the penis in a rigid state.
The French surgeon Ambroise Pare suggested an "artificial penis" made of wooden pipe or tube for patients after traumatic penile amputation in order to facilitate a proper micturition in the standing position. Although not intended for sexual activities, one might call this device a 16th century "penile prosthesis". As per definition a prosthesis replaced the whole organ or part of the body. On the other hand on should always confine to the term "penile implant" when referring to the modern devices discussed.
The first real penile implant to facilitate an erection was used in a phalloplasty procedure performed by the Russian surgeon Nikolaj A. Bogaraz in 1936. He used the patient's rib cartilage and in later years, he even performed this operation in patients with a morphologic intact penis, but suffering from erectile dysfunction.
The first alloplastic material for the treatment of erectile dysfunction was implanted in a single patient in 1949 using an unpaired acrylic subcutaneous implant by Goodwin and Associates. Robert A. Loeffler and R.O. Pearman both also implanted acrylic rods directly to the tunica albuginea in the 1960's whereas the Egyptian plastic surgeon G.E. Beheri was the first to place the implants into the corpora cavernosa. In addition to providing a treatment for erectile problems, the introduction of the semirigid rod and inflatable implants sparked interest in studying the mechanisms of an erection, the anatomy of the penile bodies and the interrelation between patient and partner in achieving satisfactory sexual compatibility. Tests were developed which could differentiate between physical and psychological causes for erectile dysfunction. Basic science advances attempting to elucidate cellular mechanisms including penile smooth muscle relaxation have occurred. Hand in hand with our understanding of these cellular mechanisms, medical treatments acting on muscles in the penis soon became very effective. Twenty years ago, intracorporal injections to relax penile smooth muscle became popular. Over five years ago, sildenafil, an oral agent which is effective in improving erections in the majority of patients not only simplified the treatment for erectile dysfunction for many men, but brought numerous patients into the fold, who otherwise would not have opted for more aggressive therapies. Two other oral medications in the class type-5 phosphodiesterase inhibitors, namely tadalafil and vardenafil are now also available. About 2/3rds of men will respond to these oral agents and another small percentage can be successfully treated with intraurethral or intracorporally injected agents. Vacuum erection devices, which were popularized in the 1980s, are also available and when medication has not been successful, these agents, as well as penile implants have been used by some patients.
In the current environment, penile implants have played a secondary role in the treatment of erectile difficulties. When medical therapy has been ineffective or contraindicated, and when vacuum devices have proven unsatisfactory or unacceptable, implants have offered a predictable and reliable way of restoring erectile abilities. Patients who present for consideration of a penile implant, are those who have been unable to use medical therapy. Patients with diabetes mellitus and those who have had radical prostatectomy for prostate cancer respond less well to the oral medications. For patients taking organic nitrates, these medicines are contraindicated. For patients with scar tissue in the erectile bodies from trauma or following priapism, or after a previous prosthesis has been removed, penile implant placement is their only option for restoring erections. In patients with Peyronie's Disease, where soft erections and curved erections make intercourse impossible, a penile implant will both straighten and strengthen the erection.
Types Of Penile Implants
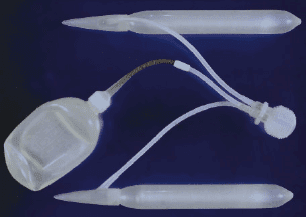
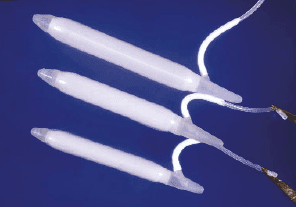
There are three classes of penile implants, hydraulic, semirigid, and soft silicone. The hydraulic consists of two types, the three piece inflatable and the two piece inflatable. In the three piece inflatable group, there are two vendors, Mentor Corporation and American Medical Systems (AMS). (Figure 1) Mentor promotes two types, the alpha I and the narrow based cylinders. Both cylinders expand in girth, but not in length. The narrow cylinder is more appropriate for the smaller penis and the penis with considerable scar tissue where dilation to a larger caliber corporal body is not easily accomplished. American Medical Systems sells the Ultrex, CX, and CXM cylinders. The Ultrex is composed of three layers. The inner layer is silicone, the middle layer is a bidirectional Dacron-lycra weave and the outer layer is silicone to prevent in-growth of tissue into the woven material. The bidirectional weave allows the cylinder to expand both in length and in girth. The CX cylinders and CMX are of similar construction, except that the middle woven layer has an unidirectional DacronLycra weave allowing the cylinder to expand in girth only. The CMX is a narrower cylinder, more appropriate for the small penis or scared corporal bodies. (Figure 2) The only two piece implant available is the Ambicor of American Medical Systems, which has two cylinders, one to be placed in each corporal body connected to a resipump which is placed through a penoscrotal approach into the scrotum. (Figure 3) There are two types of semi-rigid rod prostheses, the malleable and the mechanical. The Accuform of Mentor Corporation is a malleable composed of braided silver wire surrounded by a silicone coat. (Figure 4) The AMS 650 and 600 M implants have a stainless steel woven core with a silicone jacket. The Jonas implant produced in Germany has a silver core and a silicone covering. The mechanical prosthesis, termed the Dura II, has articulating segments of polyethylene held together by a central spring and is now sold by American Medical Systems. (Figure 5) These articulating segments are covered by a polytetrafluoroethylene sleeve surrounded by a silicone outer jacket to prevent ingrowth of tissue into the prosthesis parts. The soft silicone implant was introduced by Subrini. Currently these devices are manufactured in France and sold under the names "SSDA" and "Virilis" in a number of countries. This implant is indicated in the presence of residual spongy erectile tissue which permits tumescence and complementary girth expansion around a central silicone support. (Figure 6) There are a few homemade rod implants present throughout the world, but none of these has been used for export to other countries.
The three piece inflatable penile implants are somewhat complex to insert, and they require a reservoir placed in the abdominal cavity. However, they do give the best rigidity and the best flaccidity since they will fill every part of the corporal bodies, just as an inner tube will fill a bicycle tire. They also give the best flaccidity, as all fluid can be drained out of the cylinder into the reservoir when the non-erect state is desired. The pumping mechanism of both the AMS and the Mentor prosthesis does require some manual dexterity, and patients who are lacking in this ability, may find it difficult to work these devices. For patients with previous complex abdominal procedures such as a kidney transplants or neobladder, the reservoir should be placed out of the pelvis in another part of the abdomen. A surgeon might consider a simpler prosthesis in these circumstances. These devices come in the largest and the smallest size cylinder and hence give the best flexibility in sizing. The two piece prosthesis, can give good rigidity and fair flaccidity, or fair rigidity and good flaccidity, but rarely good rigidity and flaccidity simultaneously. The device however, is advantageous if the hydraulic device is preferred, but the abdominal cavity needs to be avoided. The long proximal segment between the proximal end of the implant and the input tube (5 cm) tends to make this tube palpable on the shaft of the penis in the extremely thin patient. The semi rigid rod implants are easy to insert and usually easy to manipulate. The tubes are especially bendable and with minimal exertion can easily be maneuvered in the upward or downward position. The wire devices will sometimes have spring-back and may not be perfectly positionable for erection or in a straight downward position. Cystoscopy in a patient with a rigid prosthesis may be difficult, but with flexible cystoscopes, this is less of a problem today. Patients with diminished sensation, such as those with spinal cord injury, have been more prone to have erosion of the semirigid rod cylinders to the exterior in the region of the glans because of the pressure of these cylinders in the face of absent sensation. The patient with sensation can feel pain or discomfort as these rods are rubbed against the undergarments; the patient without sensation may not appreciate that the rods are wearing through.




In the decade prior to the introduction of Sildenafil (Viagra) in 1998, sales of penile prostheses varied between 20,000 and 30,000 per year world-wide. In the latter part of 1998 and in 1999, sales plummeted to the range of 12,000 per year. More patients were now coming in to doctors offices for treatment of erectile dysfunction, .and choosing medications. We are now seeing implant sales approaching the pre-Sildenafil era rising to the range of 18,000 per year. 75% of the sales of penile implants are in the United States. 70% of the market in the USA is the 3-piece inflatable, while 20% goes to the Ambicor with the remaining 10% semi-rigid rods. Outside the United States, the inflatable market is about 60%, the rod market is about 40%.
Selection Of Patients - Informed Consent
A patient would be considered a good candidate for a penile prosthesis if he has failed medical therapy or if medical therapy was contraindicated. Patients are usually advised to try to at least consider a vacuum device before a penile implant. Patients who opt for the implant usually are highly motivated to continue with sexual activity. The patient is usually offered the choice of an inflatable, semi rigid or soft silicone implant, guided by the surgeon's advice related to his body habitus and manual dexterity. Patients with a larger penis will be best served by a three-piece inflatable. These devices tend to give the best rigidity, especially in the longer phallus. Patients with limited manual dexterity or those who would have difficulty manipulating the hydraulic devices are best encouraged to choose a semi-rigid rod or soft silicone implant. The patient should be advised that the size of the penis will likely be shorter than the original erection was. When the penile implant is in place, a sheet of scar tissue forms around the cylinders as the body's healing reaction. The scarred sheath does not stretch as the device is inflated as the natural tunica albuginea would stretch. Hence, elastic qualities of the tunica albuginea are negated by this inner sheath of scar tissue. Sensitivity of the penis, ejaculatory abilities, and sexual drive are usually unchanged following placement of the prosthesis. The patient should also be advised that the function of the implant is to make a firm and soft or bendable penis only. The devices do not restore any special sensitivity or sexual drive that may have been present years ago. When an implant is placed, the spongy tissue is pushed to the periphery to make room for the cylinders. If the cylinders are removed at a later date for whatever reason, the space will fill in with scar tissue, which will not respond adequately to other treatments such as medication or a vacuum erection device.
Pre-Operative Preparation
It is recommended that the patients bathe the genital area with a strong soap for a few days prior to the surgery. Shaving of the genital area is performed in the operating room to minimize the chance of nicks in the skin being colonized by bacteria with prior shaving. Open sores on the penis, or comedones should be treated or removed prior to the surgery to avoid these being a source of contamination during the procedure. Bishop and Associates found that patients with diabetes mellitus whose blood sugar was in better control for a period of time preoperatively as manifest by a normal hemoglobin A1C, were less prone to develop a penile implant infection than a group whose hemoglobin A1C was abnormal. A larger series reported by Wilson and Associates found no difference in infection rates with penile prosthesis placement in those with a normal or an elevated level of hemoglobin A1C preoperatively. The urine culture should be negative if possible. Patients who are prone to develop urinary tract infections such as those with a neurogenic bladder should be placed on antibiotics for a number of days prior to the surgery to maintain sterile urine. The urinary tract is usually not invaded during the placement of the penile prosthesis, although spilling of urine onto the operative field during the procedure is a possibility. Antibiotics are usually started prophylactically one hour prior to the procedure. The decision of which antibiotics to use is usually made by the surgeon, and are those antibacterials which are appropriate for treating infections due to skin contaminants. The antibiotics are usually continued for 48 hours postoperatively, at which time the wound is sealed. Some surgeons will prefer to maintain antibiotics for a week after surgery. A catheter is sometimes used to identify the corpus spongiosum during the procedure and may be removed at the conclusion of the operation or continued for up to 24 hours in the postoperative period.
Some surgeons will opt to use drains at the conclusion of the procedure to reduce the edema and to provide an exit for any bleeding which may occur in the immediate postoperative period. These drains are usually removed a day or two following the surgery. Pain following placement of a penile prosthesis is variable depending upon the patient's tolerance and the particular disease process. The pain is usually more prolonged than that associated with an operation of the same magnitude, ie., inguinal herniorrhaphy or appendectomy. Patients relate that the pain usually improves each day and that by 3-4 weeks, most of the pain has subsided. Patients are taught to operate the hydraulic devices at about six weeks. Some surgeons prefer to begin cycling these devices at four weeks, but in many patients pain may still be present to the degree where it would make such a maneuver uncomfortable. At six months, most patients relate that they hardly notice any pain present. Especially in cases of neuropathy, pain may persist beyond six months. If prolonged pain does occur, especially if the pain is unchanging or worsening, then the suspicion of an infection associated with the prosthesis should be entertained. When the patients are taught to operate the hydraulic devices, they are advised to cycle them regularly. Every week, the patient should inflate the device completely to avoid cylinder cavity contracture. They are advised to completely deflate the device daily, to avoid scar formation over the reservoir which would limit its expansion. When the patient leaves the cylinders semi-inflated for prolonged periods of time, a capsule forms over the reservoir in the collapsed state which will restrict its expansion in the future.
Incisons
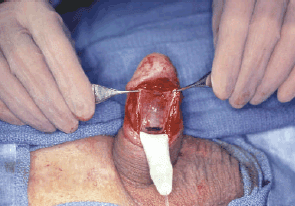
The inflatable prostheses are usually placed through an infrapubic or a penoscrotal incision. The advantage of the infrapubic incision is the secure placement of the reservoir in the midline location. If the midline prepubic area is scarred or a renal transplant is present, the epigastric extraperitoneal or intraperitoneal placement of the reservoir can be accomplished.18 If a prosthesis is placed through an infrapubic incision on the dorsal surface of the corpora cavernosa, care should be taken to avoid damaging the neurovascular bundle which runs between 11 o'clock and 1 o'clock on the upper surface of the corporal bodies. Making corporotomies at about the 10 o'clock or 2 o'clock position will avoid damaging this structure. The sensory nerves to the end of the penis and the glans run through the neurovascular band, and it is important to avoid damaging these nerves. By doing so, good sensitivity to the distal penis should be maintained after the surgery. With the infrapubic approach, the pump tubing is placed around the side of the penis into the scrotum and the pump is not usually secured in position. Migration of the pump may occur and the patient is encouraged to push the pump inferiorly each day in the immediate post-op period to assure optimal positioning. During placement of a hydraulic implant through a penoscrotal or transverse scrotal approach, the reservoir is placed blindly through the inguinal canal. Care should be taken in this approach to place this part medially to avoid injury to the iliac vessels. Decompressing the bladder will minimize the chance of injuring this structure. The advantages to this approach are the secure placement of the pump in the scrotum and the fact that the skin is not violated in the prepubic area, for a more acceptable cosmetic result. The Ambicor prosthesis can only be placed through a penoscrotal approach. The tubing from the pump to the cylinders, which is preconnected will not reach into the scrotum if this device is placed through an infrapubic incision. The semi rigid rods and soft silicone implant are commonly placed through a subcoronal, penoscrotal or ventral penile incision. A ventral incision is used in the uncircumcised patient. If a subcoronal incision is used simultaneous circumcision is recommended. If the excess foreskin is left following the closure, maceration of the suture line or lymphedema may develop. Through the subcoronal approach, there is also less tissue to close over the suture line of the corporotomy. When the penoscrotal approach is used to place semi rigid rod implants, it may be difficult to bend the rods to fit under the distal edge of the corporotomy. Extending the corporotomy may be necessary under these circumstances. In the ventral penile approach, a proximal midline skin incision is made on the ventral surface of the penis. This is retracted distally using a vein retractor and relatively distal corporotomies are made (Figure 7). The distal end of the corporotomy can then be lifted over the end of the rod using a vein retractor, avoiding the need to bend the rod. The layered subcutaneous tissue and skin closure can then be performed without overlapping suture lines. The corporotomy closures are lateral and the skin closure is in the midline.

Anesthesia
Penile implants can be placed under general or regional anesthesia. For the placement of semi-rigid rod or soft silicone cylinders, a penile block is performed with a local anesthetic. A tourniquet is then placed around the base of the penis as if one were performing an artificial erection. About 25 ccs of 1% Lidocaine is then instilled into either corpus cavernosum, held in place with the tourniquet for one minute and the tourniquet is then released. The local anesthetic then diffuses to the proximal part of the corpora anesthetizing the whole of both corporal bodies. With the placement of hydraulic implants, a penile block combined with a pudendal block has been successful. Most surgeons prefer to place these devices using general or spinal anesthesia. These blocks are sometimes not as effective or optimal as one would wish and many times must be supplemented by the injection of local anesthetic into the parts to be incised or dilated.
Operative Technique
The critical portion of the surgery is appropriate cylinder sizing. If a cylinder is larger than the corporal body can accommodate the patient may have persistent pain, protrusion of cylinders far into the glans, or curvature of the penis when it is erect. The rigid rods should be sized about 1/2 cm less than the measured length of the corporal body. This will allow comfortable bending and less springback phenomenon. With most inflatable cylinders, the cylinder of the same size as the measured corporal length should be implanted. The cylinders which expand distally (Ultrex) should be sized slightly shorter than the measured corporal length, perhaps 1/2 to 1 cm. As the cylinder expands distally during inflation, it will easily make up the difference in length and fill out the distal aspects of the corporal body to give good support to the glans. In addition to length sizing, proper width fit is critical for optimal support for the erection. Models of the three-piece inflatable, the Mentor and the AMS CX come in two widths. The narrow-width cylinders with modest inflation are 9.5 mm in diameter. Upon full inflation, they will expand to at least 14 mm in girth. The wider versions, when expanded to modest inflation are 12 mm in diameter and when fully expanded are at least 18 mm in girth. The optimal width fit of an inflatable cylinder is that which fills the corporal body in a finger in glove like fashion. Hence when the corporal body is relatively narrow, a narrow cylinder will give equally good rigidity as a larger cylinder with less discomfort and less possibility of causing penile deformity. The technique to determine whether the wider or narrower cylinder would be more appropriate in a particular patient is to assess the ease with which the dilator passes during dilation of the corporal body. If the 12 mm dilator passes with some snugness, it would be more appropriate to use the narrower cylinder rather than the wider cylinder under the circumstance as it would give equally good support with less potential for problem. The semi-rigid rods, the soft silicone device and the Ambicor implant are sold in fixed-width sizes. Deciding which size of these devices to implant would be appropriate before opening the sterile package. The simple technique to determine which size would be more appropriate would give the better fit would be to place two dilators of the proposed size simultaneously, first distally, then proximally into the corporal bodies. One then apposes the thumb to the index finger between the two dilators (Figure 8). If there is wide separation of the dilators ie., if one is able to appose the thumb to the index finger between the two dilators, then that particular size would be too narrow and a larger size would be more appropriate. An ideal fit would be achieved if one were to obtain a slight separation of the dilators as the thumb is apposed to the index finger. If there is no separation of the dilators as this maneuver is performed, then a tight fit would be achieved with that particular size cylinder.

The inflatable cylinders have an input tube which exits from the cylinder at the proximal location. This tube may run intracorporally and exit at a convenient location from the corporotomy or may exit directly where the tube comes off the cylinder. In some previously constructed cylinders, if this tube rubbed against the cylinder, input tube wear would occur. However, the current model cylinders with the polyurethane of the Mentor and the triple layer of the AMS 700 and Ambicor have eliminated this wear feature. Either technique allowing the tubing to exit directly where it comes off the cylinder or allowing it to run intracorporally is appropriate and is the surgeon's choice. Caution should be noted with either technique. If the cylinder is allowed to run intracorporally and extensive scar tissue is present in the corporal body, one should determine that inflation and deflation of the cylinder readily occur. The scar tissue may be so dense that once the cylinder is inflated, the input tube may be compressed, even though it is the non-kink type. Under this circumstance inflation would be possible, but deflation would be impossible. If this did occur, one should incise the corporal body over the tubing so that the tube exited the corporal body as it came off the cylinder. If one allows the tubing to exit the corporal body as it comes off the cylinder, it should not be so far distal that it would be sheared during the pressure exerted during intercourse. It also should not be too far proximal as the corporotomy closure would be difficult due to poor exposure.
An adequate reservoir cavity should be created to minimize the chance of autoinflation. Auto-inflation occurs when the cylinders of a hydraulic penile prosthesis do not stay deflated. The implant patient has a chronic partial erection sometimes causing embarrassment and discomfort. This problem is caused by abdominal pressure or a tight reservoir cavity forcing fluid from the reservoir into the cylinders. If autoinflation persists, the condition becomes generally irreversible and in need of surgical intervention to expand the reservoir cavity. The body reacts to any foreign body by surrounding the object with a fibrous capsule. All components of a penile prosthesis are surrounded by such a sheath. Earlier series reported the incidence of auto-inflation in 11% of patients with 2% requiring operative correction.21 Mentor Corporation has introduced the "lock-out valve" to prevent the occurrence of auto-inflation (Figure 9). The lock-out valve works by responding to fluid pressure changes in the tubing to the prosthesis and not to pressure from the reservoir.

The apical location of this valve modification allows fluid to flow bi-directionally. During cylinder deflation, the valve opens to positive pressure in the tubing. During cylinder inflation when the collapsed pump bulb recovers, negative pressure opens the valve. The fluid in the reservoir flows in and out due to prosthesis fluid pressure. There must be negative pressure from the pump side for the fluid to flow from the reservoir. Elevated reservoir pressure, such as that due to the Valsalva maneuver, does not result in fluid flow from the reservoir. Follow-up with this reservoir modification has been excellent. When placing the reservoir, care should be taken to avoid placing the lock-out valve against a firm structure such as hard scar or bone. This may indent the valve causing it to malfunction. The usual location for the reservoir is the prevesicle space, either placed through a midline incision or through the inguinal canal. If this area however is excessively scarred following pelvic surgery, then the reservoir can be placed in an alternative location, such as within the peritoneal cavity. If this is done however, the reservoir should be placed against the pelvic wall and not allowed to float freely within the abdominal cavity. The bowel can readily be intertwined around a reservoir floating freely in the peritoneal cavity which can result in bowel obstruction. In addition, there should be no pressure on the tubing pulling the reservoir against a viscus as erosion of the reservoir into bowel and bladder has been reported. The circumstances in which this has happened have been those in which there has been pressure pushing the foreign body against the wall of the viscus. In addition to the peritoneal cavity an extrapelvic location of the reservoir is also an option. The epigastric placement of the reservoir is certainly appropriate and this can be accomplished by an upper abdominal incision, incision of the aponeurosis of the external oblique with separation of the internal oblique and transversalis muscle fibers. Preperitoneal placement is possible and the tubing can then be tunneled down to the prepubic or scrotal area for connection with the tubing leading to the pump. This location is also appropriate for placement of a three-piece prosthesis in renal transplant patients or those awaiting transplant. This will obviate the need for dealing with prosthetic parts or reservoir when operating on the transplanted kidney. Fluid placed in the reservoir should be slightly less than the reservoir capacity, but at least 10 ccs more than the volume of the inflated penile cylinders. This will permit some expansion of the cylinders which may occur as scar is stretched in the postoperative period.
With the infrapubic approach, the prosthesis pump is placed freely in the scrotum after an adequate subcutaneous pocket has been created. A large Hegar dilator, size 20, has proven helpful in achieving an adequate space for pump placement. The pump should be placed anterior to the testis and as far inferiorly in the scrotum as possible. Patients are encouraged to push down on the pump gently in the first few weeks in the postoperative period to maintain this dependent position. If it migrates to the location adjacent to the shaft of the penis, it becomes difficult to operate and inconvenient during intercourse. When the scrotal approach is used, the pump can be fixed in its location by bring one or more of the tubes exiting the pump through the scrotal septum to prevent the pump from twisting or migrating during the postoperative healing. During the placement of a penile prosthesis, copious irrigations with antibiotic fluid should be stressed. Every five minutes the field is flooded with these irrigations, instilled under force with an Asepto syringe. At the conclusion of the procedure, two layers of subcutaneous and a layer of skin closure are recommended over any prosthetic parts.
Results
Thesis introduced over 30 years ago were relatively common. One report cited 50% repairs in 5 years following implantation. Manufacturers have eliminated or reinforced areas which have tended to wear, and the products we are seeing today have reliability rates equal to or greater than other mechanical products. In addition, surgeons have gained experience over the years in implantation techniques and proper sizing and placement of parts. A number of recent series have been published which attests to this fact. Milbank and his colleagues have reported a mechanical survival rate at 5 years of 78% using the Ultrex penile implant. Levine, Estrada, and Morgentaler reported 93% survival at 31/2 years with the Ambicor prosthesis. Choi reporting on the reliability of the AMS 700 CXM prosthesis in Asian men, related that 90% were working well at 5 years. Carson, Mulcahy, and Govier reporting in a prospective study on the AMS 700 CX showed an 86% mechanical survival at 5 years. Wilson and his colleagues related that 93% of the enhanced Mentor Alpha I prosthesis were still working well after 5 years following implantation. Govier and coworkers reported that 91% of their prostheses were working well at 3 years. A number of different types of implants were reported in this series 29°. Debocq and colleagues related a series with a mean followup of 51/2 years, which showed that the Mentor Alpha had a 96% survival while the AMS 700 Ultrex and CX had an 84% survival. In late 2000, American Medical Systems introduced parylene micro coating as a feature to enhance the 700 series' cylinder durability and subsequent longevity. Parylene coating is applied via a vapor deposition process, to non-tissue-contacting surfaces only and increases lubricity to the silicone surface, hence reducing friction and wear. This micro-thin (60 millionths of an inch) parylene layer, has been demonstrated in bench testing to add millions of fold and tube wear stress cycles before detectable wear is measured on both sides of the inner tube cylinder component and the inside of the outer tube cylinder component. This feature is expected to further reduce the incidence of revisions with the 700 series inflatable implant. In addition to improving product longevity, this innovation maintains cylinder flaccidity and functionality. Repair rates in the range of 10-20% within the first 5 years are to be expected and when counseling patients, these figures may be quoted.
Implant Repair
In the United States, all penile prosthesis sold now have a lifetime warranty. When approaching a patient who needs a repair, one should keep this in mind. A prosthesis which has been in place for a number of years, ie., two years or more and certainly more than 5 years should be entirely replaced. This provides the extended wear time on all of the parts in place. If the prosthesis develops a malfunction within a few months of placement, consideration should be made to leave in parts which are not defective. This is particularly applicable to the penile cylinders. When the corporal bodies are opened to replace cylinders, scar tissue forms which in time will contract. Patients who have had a number or repairs relate that after each change of cylinders, the penis has become noticeably shorter. If the surgeon plans on leaving parts of the device behind, the first parts of the prosthesis inspected are the connections. These are usually in one location and the connection should then be dissembled and the volume of fluid in the reservoir determined. Each of the parts can then be tested using an ohmmeter. With this technique, the part to be tested is filled with saline. A blunt metal needle is then placed into the tubing leading to that particular part. One limb of the ohmmeter cable is placed on the metal needle, the other limb is placed on a retractor located in another part of the wound. A deflection of the ohmmeter needle would indicate that current is passing from that part to the retractor, ie., there is a leak in that part and sodium chloride ions are passing through the defect to complete the circuit (Figure 10). That part should then be replaced. If no deflection of the ohmmeter needle occurs while testing a particular part, this would indicate that the wall of the part is intact and sodium chloride irons are unable to pass from the interior of that part to complete the circuit to the retractor in the wound. Filling parts of the implant with contrast material and then checking for extravasation with an x-ray has also been used to detect the site of leakage. When incising scar tissue over the tubing electrocautery is helpful. The setting should be less than 35 watts. Higher currents will not damage the silicone, but will be detrimental to the polyurethane coating of the Mentor device. For repairs, it is important to check for the presence of infection. Recent reports have indicated that on revisions the infection rate is higher than it is with initial implants. The Incidence of positive cultures taken from the wound during repair is also significantly high, even in the absence of signs of infection. For this reason some surgeons are now copiously irrigating the wound of revision cases with additional antiseptic solution such as hydrogen peroxide and Betadine in addition to the antibiotic irrigations used on all prosthesis cases. Upon placement of the cylinders in revision cases, one should re-measure the length of the corporal bodies. Longer or shorter cylinders may be more appropriate in the particular circumstance.

Scarred Coporal Bodies
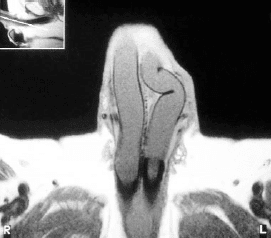
Peyronie's Disease is a common condition in which scar replaces the natural elastic covering of the corporal bodies. This is usually a focal scar which results in curvature of the penis towards the side of the scar as the tunica albuginea no longer expands in this area. If hydraulic penile implant cylinders are to be placed in scarred corporal bodies, the Ultrex type should not be used. This tends to expand distally, completely filling the end to corporal bodies and not allowing the ends to shift over the body of the cylinder. If the AMS CX or the Mentor cylinders are used which do not expand distally, then the corporal bodies can shift over these cylinders and the intrinsic rigidity of the cylinders will usually straighten the penis very adequately. If one has used Ultrex cylinders and finds that curvature of the erection when these cylinders are inflated occurs, they should be switched to the CX variety, which will usually straighten the penis very adequately. If hydraulic cylinders are placed and significant curvature of the penis persists, then a modeling technique described by Wilson and his colleagues can be tried. With this technique cylinders are inflated to maximum. The tubing leading to the cylinders is then clamped and the cylinder is forcibly bent against the curve and held for 90 seconds. A feeling of the scar tearing can sometimes be appreciated during this maneuver. The cylinders are then reinflated to determine if straightening has been achieved. If significant curvature persists despite this initial modeling maneuver, then the modeling can be repeated. A high percentage of curved erections can be straightened using this technique. One should then maintain the penis in the semierect position for two months following this procedure to allow the scar to heal in the straight position. The corporotomy closures are checked for rupture and the urethra is inspected for injury as this has been reported during this modeling maneuver. If modeling has failed to straighten the penis, then a formal straightening procedure can be performed. The Nesbit technique has been used successfully in this regard. Using this operation, elliptical wedges of tunica albuginea are removed from the convex surface of the curve. The cautery device is useful for this purpose and will avoid damaging the prosthesis with a sharp instrument. The edges of the tunica albuginea are then approximated using long term absorbable suture such as PDS. An alternative procedure would be to incise the concave or inner surface of the curvature. The cylinders are then inflated and the wedge-shaped defect is obvious. This defect can then be covered using graft material. A Gortex or Dacron graft was used for this purpose and permanent suture was employed to attach the graft to the tunica albuginea. Recently SIS (porcine small intestinal submucosa) and Tutoplast (cadaver pericardium) which are more natural materials have been used very satisfactorily. If the latter materials are used a long term absorbable suture can be used to attach the graft to the tunica albuginea. A 10% larger size graft than the gap should be used when these natural materials are employed due to contracture of the graft over the long term. Occasionally the circumstance is encountered where the wall of the tunica albuginea is inadequate to completely cover the prosthesis cylinders without excessive tension. This could follow resection of the tunica, or a situation where excessive scar tissue will not enable the surgeon to close the tunica over the prosthesis without severely narrowing the corporal cavity. In this case, these graft materials, either synthetic or natural may be used to reinforce the wall and replace the wall to give complete covering of the cylinder and adequate caliber to the corporal body (Figure 11) The technique of placing these grafts is similar to that described for straightening the erection with the cylinder in place. Austoni et.al. used a variety of grafts as strips placed to fill longitudinal incisions in the tunica albuginea to broaden the caliber of the corporal bodies enhancing girth in association with hydraulic implant placement (Figure 12). A narrow caliber of the corporal body can be made larger using the Otis urethrotome to incise the scar sharply or various cavernotomes which shave slivers of scar as the instruments are maneuvered backward and forward. Deformities or malposition of implant cylinders can usually be detected by palpation of the penile shaft. However, if palpation does not give a definitive answer, MRI (Magnetic Resonance Imaging) of the corporal bodies will clearly delineate the location and shape of the cylinders (Figure 13).




Corporoplasty - Glans Fixation
Protrusion or extrusion of penile prosthesis cylinders distally out of the corporal body is unusual (Figure 14). Circumstances which may dispose to this are aggressive distal dilation during placement, over sizing of cylinders, ie., placing wider cylinders, where narrower cylinders may be more appropriate, or excessive pressure against the end of the penis during sexual activity. The protrusion can be repaired using a natural tissue method. A hemi-circumcising tissue is created on the side of the extrusion. A longitudinal corporotomy is made over the cylinder and the cylinder removed from the cavity. The back wall of the sheath that contained the cylinders is then incised and a new plane developed behind this wall down to the distal end of the corporal body (Figures 15-16). This original back wall will now provide the outer covering of the penile prosthesis cylinder. The cylinder is then replaced into the newly created cavity and the outer wall reinforced, closing the original tunica albuginea and adjacent scar tissue with longterm absorbable suture (Figure 17).

An alternative approach would be to place a windsock of synthetic material over the end of the prosthesis and to replace it into the corporal body as a reinforcement for the distal tunica albuginea. This substitutes one foreign body close to the skin surface for another. Carson compared the two techniques natural tissue repair versus windsock and found that the former was more successful. After corporoplasty the glans may be excessively mobile. Glans fixation may be necessary. In addition, in certain patients following penile prosthesis placement, the glans is noted to be hypermobile, either dorsally, ventrally or in either direction, a condition called SST deformity or floppy glans. A circumcising incision can be made and the tissue under the glans dissected free. A nonabsorbable 3-0 suture can then be placed through the glans substance and through the end of the tunica albuginea over the end of the inflated cylinder. The suture is tied securely. The glans is then fixed against the end of the prosthesis cylinder. This can be done in one quadrant, or all four quadrants as needed to securely fix the glans and prevent excessive mobility.
Infection
Infection associated with a penile prosthesis is considered a catastrophic event necessitating removal of the device. Today, the rates of infection are low in the range of 1-3%. Infection associated with the prosthesis should be considered if the patient has persistent pain beyond two months following the surgery. This would be especially true if the pain is unchanging or even increasing with time. The presence of fever or erythema in the wound with fixation of parts such as the pump to the overlying skin would also be signs that would lead one to suspect an infection being present. If persistent purulent drainage occurs from the wound, especially if this is increased when pressure is placed on parts of the prosthesis such as the cylinder or pump, or if any part of the prosthesis is exposed, this would indicate an infection is present. The use of systemic antibiotics in an attempt to clear such an infection has not been successful. Many organisms which are associated with a penile prosthesis infection produce a biofilm or slim which surrounds the prosthesis parts. This inhibits phagocytosis and provides a barrier to diffusion of antibiotics to the area where the organisms are present. It virtually provides a hiding place for the bacteria. When one is convinced that an infection is present, it is prudent to explore the wound and remove all the implant parts and foreign materials. This would include suture material and any graft material used to rebuild parts of the penis associated with prosthesis surgery. The traditional approach has been to return in 2-6 months, when the infection has cleared to replace a new prosthesis. In this circumstance however, the erection will be noticeably shorter, perhaps 1-2 inches and the placement of the implant cylinders would be more difficult because of development of scar tissue in the penis after infection and cylinder removal. An alternative has been advocated and is gaining popularity, termed a salvage or a rescue procedure. This entails removal of all implant parts and foreign material, cleansing the wound with a series of antiseptic solutions and replacing the prosthesis at the same procedure.
Salvage protocol used for infected penile implants:
- Remove all prosthetic parts and foreign material.
- Irrigate wound with seven antiseptic solutions.
- Change gowns, gloves, surgical drapes and instruments.
- Insert new prosthesis.
- Close wound with no drains or catheters.
- Oral antibiotics for one month.
Antiseptic irrigating solutions used during salvageprocedure:
- Antibiotics
- Half strength hydrogen peroxide
- Half strength Betadine
- Pressure irrigation (water pic) with 1 gm Vancomycin and
- 80 mgs of Gentamicin in the 5 liter irrigating solution
- Half strength hydrogen peroxide
Long-term follow-up has shown that this has been successful in about 84% of cases. This alternative is less successful when the tissue surrounding the implant as well as the implant cavity is infected. This usually occurs soon (1-2 months) after the original surgery for placing the implant when a considerable amount of cellulitis is evident in the wound with or without abscess formation. In these circumstances the use of systemic antibiotics (vancomycin-gentamicin) for 48-72 hours prior to the salvage has improved the chances of success. An obvious abscess or fluctuance should also be drained prior to salvage procedure. If fluid is available for culture, the organisms involved can be determined and more appropriate antibiotics substituted systemically for 48-72 hours prior to initiating a salvage procedure. Improvement or resolution of cellulitis suggests that the chance of salvage succeeding would be higher. The advantage of the salvage procedure is that most of the length of the penis will be maintained. In addition, it is easier to place cylinders while the cavities in the corpora cavernosa are open, rather than returning at a later date to create new cavities in scar tissue.
A delayed form of salvage has been advocated. Using this technique, the prosthesis is removed and drains are placed in the wound though which antibiotics can be instilled for about 72 hours. The organisms involved in the infection are certain and more appropriate antibiotics can be substituted if necessary prior to drain removal. The patient is returned to the operating room after 72 hours and a new prosthesis is placed at that time. Delayed salvage involves a longer hospitalization and two operative procedures and is definitely more costly. In addition after three days of an inflammatory process, wound closure may prove difficult, especially in the very thin patient. Success with delayed salvage is similar to that of immediate salvage, and the immediate salvage has become the preferred method.
Contraindications to salvage include tissue necrosis, patients who are severely ill, such as those with lifethreatening conditions such as ketoacidosis or sepsis, and those patients in whom bilateral urethral erosion of the prosthesis cylinders has occurred.
Experimental studies in Sprague-Dawley rats by Dhabuwala and Associates demonstrated that coating silicone graft material with antibiotics, particularly rifampin/minocycline, reduced the incidence of graft colonization in contaminated wounds. Minocycline and rifampin have been safely used as a surface treatment in indwelling venous and urinary catheters. It has been demonstrated to be an effective method to provide broad-spectrum inhibitor activity against gram-positive and gram-negative bacteria. This combination is particularly effective against Staphylococcus.
In May 2001, American Medical Systems introduced InhibiZone antibiotic surface treatment of its three piece inflatable implants. InhibiZone is a formulation of minocycline and rifampin, which is impregnated onto the outer surface of the prosthesis, resulting in a mottled orange-yellow covering (Figure 18). Antibiotics impregnated into the device surface elute from the silicone matrix when exposed to a warm, moist environment. Concentrations represent less than a common oral or IV dose. Of theoretical importance, local antimicrobial release will prevent early colonization and the development of a bacterial biofilm layer.
The mechanism of antimicrobial activity of minocycline (inhibits protein synthesis) and rifampin (inhibits DNA-dependent RN polymerace) may help reduce the likelihood of developing bacterial resistance to either agent. In-vitro and in-vivo studies have demonstrated that minocycline is effective in retarding the emergence of staphylococcal strains that are resistant to rifampin. Minocycline and rifampin also benefit from not commonly being used in the hospital setting, which may reduce the risk for bacterial resistance developing. In the largest single clinical experience with InhibiZone, Wilson reported on 234 total inhibiZone implants with follow-up of up to 18 months, 73.1% original (n=171) and 26.9% revision (n=63). There were no infections in the original series and a 1.2% infection rate (n=3) for the revision series. However, there were no staphylococcal infections and all organisms cultured (Enterococcus, Streptococcus, Candida) were resistant to the minocycline/rifampin combination.


In another local approach to prevent bacterial colonization and infection, Mentor Corporation has developed a proprietary hydrophilic coating that inhibits bacterial adherence. A number of recent publications have reported on the efficacy of antibiotic-soaked, hydrophilic-coated substrates.
In a recent study in rabbits, the ability of the new hydrophilic coating was investigated for its ability to prolong the effect of intraoperative antibiotics. Coated and uncoated discs were soaked in antibiotics and the zones of inhibition against 4 microorganisms were studied at various time points from 0 to 5 days. There was statistical benefit in limiting bacterial growth of the coated samples for up to 3 days, especially against Staphylococcus epidermis, the most common organism associated with implant infection. In theory, the anti-adherence properties and the ability to absorb water-based antibiotics will reduce the chances for infection. Mentor Corporation introduced its hydrophilic-coated prosthesis (Titan) in the fall of 2002 (Figure 19). Early follow-up has suggested a clinical benefit for patients implanted with the Titan in regards to reduced infection rates. An important caveat is that the introduction of any new microbe-resisting coating should not allow an implanting surgeon to reduce his vigilance, sterile technique, and use of antibiotics to prevent implant infections. Despite the early reports of benefit from these innovations, a larger number of implantations will need to be performed by a number of different centers and surgeons, followed over time, and analyzed in order to demonstrate statistically a benefit.
Satisfaction
Of all the currently available treatments of erectile dysfunction, the penile implant has the highest satisfaction rate. It is the most invasive and least often chosen option, but once these devices are placed, patients and partners are gratified in the vast majority of cases, with the resulting erection. Levine, Estrada, and Morgentaler, reported that 96% of patients and 91% of partners were satisfied with the results of the Ambicor prosthesis. Montorsi in a series of 185 patients from a number of institutions reported on the AMS 700 penile prosthesis with a 98% patient satisfaction rate and 96% partner gratification. In a multi-institutional report from Taiwan, where a number of prostheses were used on 331 patients, 87% of patients were satisfied with the result. A multi-institution report from Italy surveyed a number of patients with penile implants and Peyronie's Disease, 79% of the patients were satisfied and 75% of the partners seemed pleased with the result. The major reason for dissatisfaction in these cases was the shorter size of the erection. Others reasons for dissatisfaction include the fact that it did not feel natural, that the sensitivity and drive were not as good as they were in younger years, and that the partner did not have as great a role in creating the erection as she once did. Satisfaction rates are considerably higher than those reported for patients taking medication or using vacuum devices to restore their erections.
Summary
Penile prostheses were introduced as the first effective treatment for erectile dysfunction over 30 years ago. They have an important role in the treatment of erectile dysfunction when medication has been ineffective or ill advised and vacuum erection devices have proven unsatisfactory. Repair rates in the range of 10-20% at five years are very acceptable and compare favorably with other mechanical products. Although they are the least chosen and most invasive treatment option, they have the highest satisfaction rate of all available options. They provide a predictable and reliable result. Virtually any patient who is motivated and medically suitable to continue with sexual activity, can be a candidate for placement of these devices.
No comments:
Post a Comment