
Given the complexity of the system, it is not surprising that a wide variety of diverse disorders may result in erectile dysfunction. Often, the cause is multifactorial, but vasculogenic causes are the most commonly implicated.
Because the development and maintenance of a rigid erection depend on achieving a high intracavernosal pressure, it is not surprising that disorders affecting the peripheral arterial blood flow are strongly associated with erectile dysfunction.
The most common cause is atheroma involving either the common or internal iliac arteries or their more distal branches. The risk factors for this are similar to those for coronary artery disease (including smoking, hypertension, hyperlipidemia, diabetes mellitus and obesity).
Narrowing or occlusion of the internal pudendal arteries reduces perfusion pressure to the corpora, resulting in a failure to achieve full rigidity. In the absence of such pressure, the normal venoocclusive mechanisms cannot operate and, thus, the problem is compounded by secondary venous leakage. Obliterative disease of the aorta may also result in erectile dysfunction.

Figure 1. An atheroma affecting both common iliac arteries results in vascular insufficiency, a major cause of erectile dysfunction.
Venous leakage
In the presence of a normal arterial inflow, normal veno-occlusive mechanisms should slow egress of blood from the corpora to a virtual trickle during full erection. Failure to do so results in a flaccid erection and leakage of blood, either into the deep dorsal vein...
| Box 1. Risk factors for erectile dysfunction: |
Vascular factors:
|
| Box 2. Vascular pathophysiology of organic erectile dysfunction: |
|
Or the cavernosal venous system (Figure 2). The etiology of this is obscure, but is more likely to be a primary disorder of intracavernosal smooth muscle than a problem primarily related to the penile veins themselves.

Figure 2. Dynamic infusion cavernosometry and cavernosography show a venous leak (arrowed) into the pelvic veins.
Intracavernosal smooth muscle fibrosis
Full erection depends on achieving complete intracorporeal vasodilatation. This, in turn, depends on normally functioning corporeal smooth muscle. Aging and/or ischemia may result in degeneration of smooth muscle cells, thereby impairing the ability to respond to vasodilator signals. During flaccidity, the oxygen saturation of the blood within the lacunar spaces is low (40 mmHg). During erection, however, the inflow of arterial blood raises the oxygen saturation of lacunar blood to >90mmHg.
The current evidence suggests that the development of intermittent erections may be an important mechanism for maintaining full oxygenation and, thus, function of cavernosal smooth muscle. Conditions of low oxygenation promote the production and release of transforming growth factor-β1. This molecule, in turn, results in the formation of collagen, with the resultant development of intracorporeal fibrosis (Figure 3). This may help to explain the physiological importance of the phenomenon of intermittent nocturnal penile tumescence. This is an important concept because it suggests that loss of erection due to any cause may be compounded by loss of cavernosal smooth muscle function and fibrosis. Clearly, such considerations may have an impact on the timing of treatment decisions in circumstances such as erectile dysfunction following radical prostatectomy.

Figure 3. Deleterious effects of low oxygen (O2) levels on intracorporeal smooth muscle. Low O2 tension promotes the release of transforming growth factor β1 (TGF-β1), which acts on TGF-β1 receptors to stimulate the production of collagen-inducing fibrosis. In contrast, high O2 tension, as occurs during nocturnal erections, stimulates the production of prostaglandin E1 (PGE1) which, in turn with forskolin, stimulates adenylate cyclase to produce cyclic adenosine monophosphate (cAMP) from adenosine triphosphate (ATP). cAMP induces and maintains healthy smooth muscle activity. PDE, phosphodiesterase; PGS, prostaglandin synthase.
Failure of intracavernosal neurotransmission
The molecular mechanisms of vasodilatation and vasoconstriction that underlie erection and detumescence have only recently been elucidated. Bearing in mind their complexity, it would be surprising if specific abnormalities of neurotransmission did not translate into clinical erectile dysfunction. As yet, however, none have been specifically described, but failure of NO production due to lack of NO synthase or abnormalities of receptor or second-messenger function may well underlie some cases. More research is needed in this rapidly evolving area.
Neurogenic Causes
The dependence of normal erectile and ejaculatory function on intact neural pathways to and from the brain has already been mentioned. Not surprisingly a considerable number of neurological disorders may result in erectile dysfunction (Box 3). Those involving the central nervous system include cerebrovascular accidents, Parkinson's disease and multiple sclerosis. Damage or degeneration of peripheral nerves supplying the corpora also results in erectile dysfunction. Examples include diabetic neuropathy, cauda equina lesions due to a prolapsed intervertebral disk, and iatrogenic neural injury during abdominoperineal resection of the rectum. The unusual, but interesting, disorder known as multiple system atrophy is characterized by degeneration of both the sympathetic and parasympathetic central and peripheral autonomic neurons, as well as of Onuf's nucleus in the sacral spinal cord (Figure 4). The result is progressive and disabling ortho static hypotension, urinary incontinence and erectile dysfunction, together with ejaculatory failure.
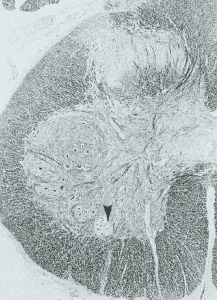
Figure 4. Histological section of the spinal cord at the level of the S2 segment shows selective degeneration of Onuf's nucleus (arrowed), which contains the cell bodies of the pudendal nerve, responsible for innervating the pelvic floor, a feature of multiple system atrophy (formerly known as Shy-Drager syndrome). Men who have this disorder often present with erectile dysfunction and incontinence.
Endocrinological Causes
Testosterone secreted from the Leydig cells of the testes under the influence of luteinizing hormone (LH) is necessary for normal male sexuality and sexual function (Box 4). Medications such as luteinizing hormone-releasing hormone (LHRH) agonists or stilbestrol, which lower circulating testosterone, result in loss of libido and in erectile dysfunction. Patients who are hypogonadal as a result of pituitary or testicular dysfunction frequently suffer from erectile dysfunction, which responds to treatment with exogenous androgens. More contentious is the suggestion that waning testosterone levels in men of middle age and beyond (Figure 5), the socalled "male menopause", are a frequent cause of erectile dysfunction and, therefore, boosting serum testosterone levels has therapeutic benefits (Box 5). However, there is some evidence from experimental animal models that androgens are necessary for the support of intracavernosal smooth muscle function and maintenance of NO synthase levels. Exogenous androgens are certainly capable of enhancing the libido, which is an important component of sexuality.

Figure 5. Progressive decrease in free testosterone levels with age. In some men, the lack of testosterone may be associated with a loss of libido and erectile dysfunction. This has been termed the 'male menopause'.
Dihydrotestosterone (DHT), the potent androgenic metabolite of testosterone produced by the enzyme 5α-reductase, is crucial for the normal development of the male external genitalia, seminal vesicles and prostate, but is not essential for either the libido or erectile function. Compounds such as finasteride, which inhibit the activity of 5α-reductase type II, result in shrinkage of the prostate by 20–30%, but have been reported to cause erectile dysfunction in only around 3–5% of patients. However, in the 4-year placebo-controlled study of finasteride recently reported by McConnell and colleagues, nearly 14% of patients taking the active drug experienced some form of sexual dysfunction.

Figure 6. Magnetic resonance imaging with gadolinium enhancement ((a) anteroposterior view; (b) lateral view) of a pituitary tumor (chromophobe adenoma). This is a rare cause of erectile dysfunction, and is usually associated with elevated levels of prolactin and diminished levels of testosterone.
Prolactin, which is released from the pituitary gland, acts as an inhibitory factor in male sexual function. Hyperprolactinemia, either idiopathic or, less commonly, the result of a tumor such as a pituitary prolactinoma (Figure 6), is associated with erectile dysfunction, as is the more common entity of idiopathic hyperprolactinemia.
Correction of the raised prolactin levels using bromocriptine may sometimes restore potency in such patients.
| Box 3. Neurogenic pathophysiology of organic erectile dysfunction: |
|
| Box 4. Endocrinological pathophysiology of organic erectile dysfunction: |
|
| Box 5. Age-related pathophysiology of organic erectile dysfunction: |
|
Priapism and Postpriapism Erectile Dysfunction
Priapism may be defined as an involuntary erection that lasts for more than 4–6 h. The condition may be spontaneous or secondary to intracavernous pharmacotherapy. Spontaneous priapism may be idiopathic or associated with blood disorders such as sickle cell anemia, leukemia or other malignancies (Figure 7).
This photo may contain content that is inappropriate for some peoples.
NOT FOR THE FAINT OF HEART!
To view this photo, please verify you are 18 or older:
After 4–6 h, a persistent erection usually becomes painful, but late presentation is not uncommon because of embarrassment. Initial therapy involves corporeal aspiration and injection of adrenergic vasoconstrictor substances such as phenylephrine or metaraminol (Aramine®). Because these potent vasoactive agents frequently enter the circulation after intracorporeal injection, blood pressure should be carefully monitored during therapy.
Although pharmacotherapy with aspiration and injection of vasoactive agents is often successful within 6–12 h of onset of priapism, beyond that time period the efficacy of any therapy is rapidly diminished. Initial high-flow priapism is followed by lower flow and progressive deoxygenation of the corpora. In these later cases, aspiration of the corpora reveals dark deoxygenated blood. Progressive ischemia to the intracorporeal smooth muscle renders the helicine arteries and walls of the trabecular spaces progressively less capable of developing sufficient vasoconstriction necessary to restore and maintain flaccidity.
The consequence of untreated priapism or priapism unresponsive to therapy is the development of corporeal fibrosis. This results in erectile dysfunction which is difficult, and sometimes impossible, to treat. Even insertion of a penile prosthesis may be technically difficult in such cases because the fibrosis renders dilatation of the corporeal space problematical.
Psychogenic Causes
Psychological causes were once widely assumed to be the predominant cause of erectile dysfunction. However, if the correct definition of erectile dysfunction is applied, namely, the persistent loss of penile rigidity in all circumstances, then psychogenic erectile dysfunction proves to be less common than its organic counterpart, especially in older men. Psychogenic erectile dysfunction typically occurs in younger men, and is variable and often associated with performance anxiety. Increased sympathetic vasoconstrictor tone and raised circulating norepinephrine levels are most probably involved. Psychogenic factors also come into play in other forms of erectile dysfunction, as failure of erection itself induces anxiety, loss of confidence and sometimes relationship difficulties. The conviction that an erection will not develop when required, therefore, becomes a self-fulfilling prophesy.

No comments:
Post a Comment